- Exchange and Networking
- Knowledge and Learning
- Advocacy
- Our topics
By Trymore Chawurura, Ronald Manhibi, Janneke H van Dijk and Gertjan van Stam
Urban Health Facilities like city clinics, larger hospitals and other health facilities are common in Africa. They contain a mix of public and private institutes. Rural Health Facilities (RHF) like rural hospitals, clinics or health posts comprise most health facilities dispersed in African countries. In those remotely located areas, public health is usually supported by institutes, like churches and companies, in addition to the government patronage. COVID-19 and digital advancements have pushed for an addition to these two categories of facilities with a third: The Electronic Health Facilities (EHF), providing access to national health systems by means of communication devices.

The digitisation process in health, where phones provide additional access to care, is similar to that of digitisation in finance where wallets or finance institutions are augmented with electronic access to funds and services. Pushed by the COVID pandemic, digitisation in education has become mainstream: it provides access to learning where physical access became hampered.
In the process towards the Electronic Health Facilities (EHFs), two main movements can be witnessed:
USAID envisions ‘country-level capacity in digital health’ as the first priority (USAID, 2020). Along with national planning, digital health is to run on national infrastructures. However, the digital platform economy features a concentration of power: Two countries (China, USA) capitalise 90% of the digital platforms globally (UNCTAD, 2019). The African and Latin American continent – together – account for 1% only (UNCTAD, 2019). The action of decentering in digitisation, therefore, becomes topical. In the words of the French president Emmanuel Macron: “The battle we’re fighting is one of sovereignty… If we don’t build our own champions in all areas – digital, artificial intelligence – our choices will be dictated by others" (rfi, 2019).
Leaders warn about the risk of unequal power distribution in digital health and its consequences (Thatcher, J. et al., 2016): “If we are to be serious about using I[nformation] C[ommunication] T[echnologies] as a way of improving the lives for people living in the developing world, we need to empower [them] to create their own designs" (Marsden, G., 2008).
Decentering expands on the term ‘polycentric’ that the UN Secretary-General positioned as a critical digital cooperation principle (UN, 2020). Decentering involves respecting local authorities, policies, regulations and requirements related to integrating digital technologies in African health systems. It acknowledges sovereignty, agency and national capacity for Africans to steer digital health in Africa.
Community engagement embeds digital health, crucial for acceptance, legitimacy, and sustainability of its emergence and continuity. It puts communities in their rightful place: as resident inhabitants with agency – stewards – and coproducers of digital health in their distinct environments. Inclusiveness blurs the roles of all participants, community members, researchers, and all national and international partners as focus shifts to seeking shared experiences, common understanding and mutual learning (AfriCHI, 2021).
“The battle we’re fighting is one of sovereignty… If we don’t build our own champions in all areas – digital, artificial intelligence – our choices will be dictated by others." French president Emmanuel Macron
The World Health Organisation provides guidance for digital health interventions (WHO, 2019). Such intervention is in need of appropriate design, production, operations and assessments in line with the environment, available skills, and culture. Agenda setting involves the communities of care seekers, communities of digital practice, and communities of digital health experts. In Zimbabwe, SolidarMed engages with relation-holders and stakeholders in the communities it serves in Masvingo province. As a result, Public Private Community Partnerships emerged to produce knowledgeable and motivated community members who convened hackathons (Hobbins, M. et al., 2018), utilized participatory video (Makamba, P. et al., 2019), engaged with health and technology experts, and became members of the Ministry of Health and Child Care’s Technical Working Groups at national level. This also resulted in a sandwich of Zimbabwean developed digital health interventions, where local developments interface with national services (i.e. Electronic Health Registration (Impilo EHR) and laboratory information systems).
"Decentering involves respecting local authorities, policies, regulations and requirements related to integrating digital technologies in African health systems. It acknowledges sovereignty, agency and national capacity for Africans to steer digital health in Africa."
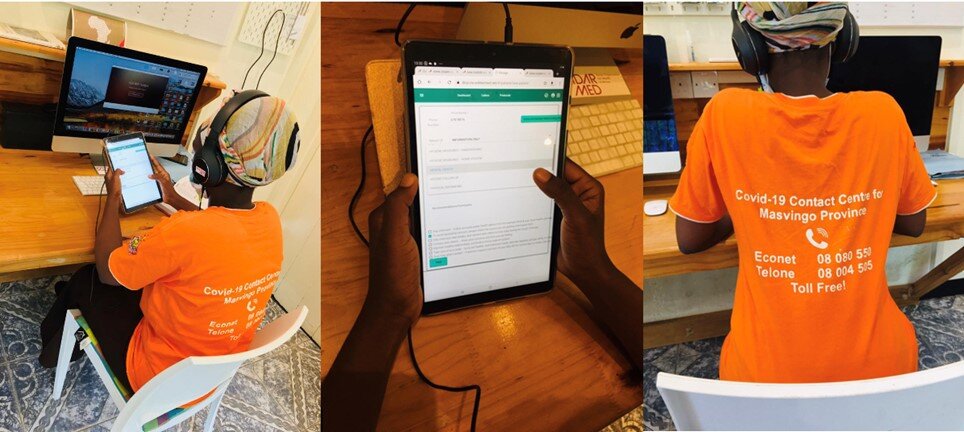
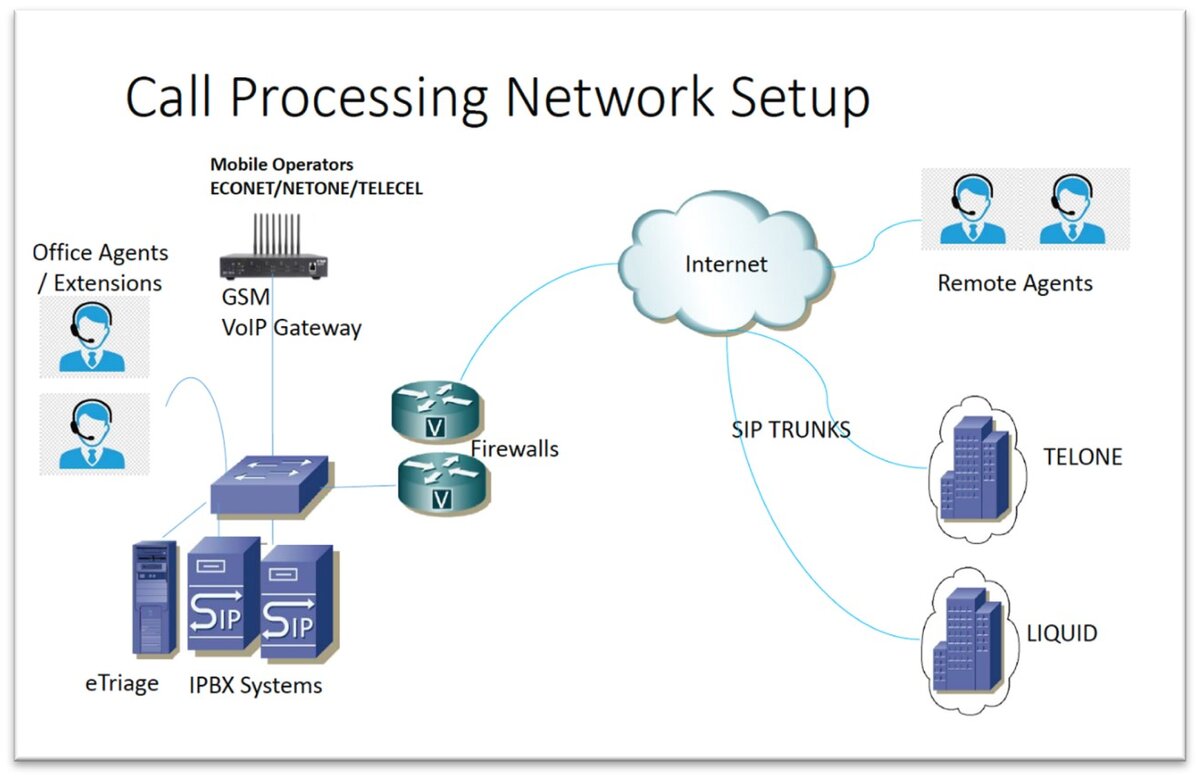
A Digital Information and Consultation Platform (DICP) was developed and operationalized in 2020, to open an additional freely accessible communication channel next to the stressed physical health facility infrastructure during the COVID-19 pandemic. With the advertisement of toll-free phone-numbers to access the COVID-19 contact centre for information and consultation in Masvingo province and nationwide, the Ministry of Health defacto commenced Electronic Health Facilities’ operations.
Digital health augments any activity in health, or in the words of the USAID leadership: “we will integrate the smart use of digital technologies into all of our health programs” (USAID, 2020, p. 2). The locally developed portfolio of digital health services in Zimbabwe consists of
The Zimbabwean government allotted over USD 4 mln to the national roll out of its self-developed and owned, open-source Impilo EHR. Many Zimbabwe-developed digital health interventions and platforms are proposed for national scale-up within the emerging national digital health strategy.
This overview shows how (sovereign) digital health platforms appear, born from community engagement and an embedded workforce. They strengthen existing health services, open new access channels, and ‘amplify what is going well’. They have also shown to continue service provisioning, access to care, even when the physical access to health infrastructure challenged due to pandemic restrictions.

"This overview shows how (sovereign) digital health platforms appear, born from community engagement and an embedded workforce. They strengthen existing health services, open new access channels, and ‘amplify what is going well’."
In the African setting, digital health needs scaffolding – where partnerships sustain engagement and workforce enhancement, local thought leadership facilitate tasks that go beyond individual abilities. These partnerships will evolve, when digitalisation ubiquitous, and when the Electronic Health Facility is enshrined as ‘business as usual’ (Cozza, M. et al., 2015). In close participatory and holistic approaches, who does what pertaining the use, design, implementation, modification, maintenance and redesign, is continuously shifting, depending on the context and political circumstances. In this setting, the narratives of thought leaders describe the experiences and understandings that become the infrastructure from which activities scale (Karasti, H., 2014).
African health systems have faced major challenges in providing equity and quality health care, especially in rural areas. The existence of these challenges has resulted in mounting interests in the potential of digital health, in a decentered manner. A reflected and carefully planned approach is needed that proceeds with diligence to involve all, leaving nobody behind.
This narrative provides a glimpse of what is ahead: a reality augmented by the emergence of Electronic Health Facilities through digitization and expanding access towards universal health coverage in Africa.